Dr. John Phillips: IVL for Calcified Below-the-Knee Lesions
The experience with Intravascular Lithotripsy in a wide variety of peripheral lesions continues to grow.
Critical limb ischemia (CLI) is the most advanced form of peripheral artery disease and often involves stenoses in calcified below-the-knee (BTK) arteries.
Dr. John Phillips, an interventional cardiologist from Ohio Riverside Methodist hospital in Columbus, Ohio has a large volume peripheral practice and has increasingly employed IVL in some of his most challenging patients. He recently posted on Twitter a CLI case involving a challenging BTK lesion and shared with us some thoughts on how IVL may increasingly be part of his CLI algorithm.
What makes calcified BTK lesions so difficult to treat?
Balloon angioplasty of the tibial arteries is the standard treatment, but outcomes can be suboptimal, particularly when heavy calcification is involved. In particular, medial calcification deeper within the vessel wall becomes increasingly more prevalent and difficult to treat. I believe it leads to decreased vessel compliance, and increased vessel recoil – a phenomenon that makes even good acute outcomes difficult to achieve.
Tell us about the case that you posted. 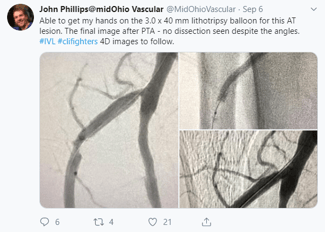
I recently treated a Rutherford Class V patient with high-grade stenosis at the ostium and proximal segment of the anterior tibial artery using IVL below-the-knee. The lesion was calcified, and we were able to confirm the degree of calcification by using 4D ultrasound. I felt that these lesions were particularly challenging, as the ostium and proximal segments of the AT have angles that often lead to dissections that can be flow limiting when standard balloon angioplasty is performed.
How was IVL helpful in this case compared to your typical plan?
IVL was quick and easy to deploy and use in this region. The actual pulsing of the lithotripsy energy is quite rapid and we don’t use long balloon inflation times (which we would with standard balloons), so the entire treatment of the lesion is efficient. We didn’t see any dissection or other complications in this region which, as I mentioned, can be quite common with other tools. The acute result looked great and it is my hope that this improvement in arterial flow gives the patient’s wounds the best chance of healing.
How do you think IVL may generally fit into your algorithm for your challenging CLI patients?
I am beginning to use IVL by itself when significant medial calcification is visible with fluoroscopy or ultrasound; or when the anatomy makes use of a different modality such as atherectomy difficult or challenging. I also routinely use IVL in conjunction with orbital atherectomy in order to create micro-fissures in advance of IVL delivery and its more macro-fissures, our “SandBlasting” technique.
Important Safety Information
Caution: Federal law (USA) restricts this device to sale by or on the order of a physician.
Indication for Use – The Shockwave Medical Intravascular Lithotripsy (IVL) System is intended for lithotripsy-enhanced balloon dilatation of lesions, including calcified lesions, in the peripheral vasculature, including the iliac, femoral, ilio-femoral, popliteal, infra-popliteal, and renal arteries. Not for use in the coronary or cerebral vasculature.
Contraindications – Do not use if unable to pass 0.014 guidewire across the lesion • Not intended for treatment of in-stent restenosis or in coronary, carotid, or cerebrovascular arteries.
Warnings – Only to be used by physicians who are familiar with interventional vascular procedures • Physicians must be trained prior to use of the device • Use the Generator in accordance with recommended settings as stated in the Operator’s Manual
Precautions – Use only the recommended balloon inflation medium • Appropriate anticoagulant therapy should be administered by the physician • Decision regarding use of distal protection should be made based on physician assessment of treatment lesion morphology
Adverse Effects – Possible adverse effects consistent with standard angioplasty include: • Access site complications • Allergy to contrast or blood thinners • Arterial bypass surgery • Bleeding complications • Death • Fracture of guidewire or device • Hypertension/Hypotension • Infection/sepsis • Placement of a stent • Renal failure • Shock/pulmonary edema • Target vessel stenosis or occlusion • Vascular complications. Risks unique to the device and its use: • Allergy to catheter material(s) • Device malfunction or failure • Excess heat at target site
Prior to use, please reference the Instructions for Use for more information on indications, contraindications, warnings, precautions, and adverse events. www.shockwavemedical.com


