Dispelling the Nodular Myths
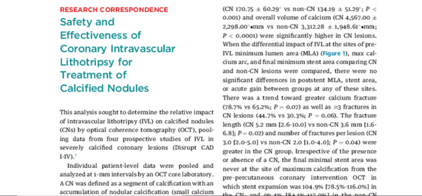
Coronary IVL Benefits in Calcified Nodules Highlighted in JACC:CI
Coming off the heels of CRT23 where Dr. Richard Shlofmitz (St. Francis Heart Hospital, Long Island, NY) presented the longer-term data of coronary IVL in calcified nodules at two years, Dr. Ziad Ali (St. Francis Heart Hospital, Long Island, NY) et al. have recently published the initial coronary IVL experience in calcific nodules within JACC Cardiovascular Interventions. Following the publication, titled, “Safety and Effectiveness of Coronary Intravascular Lithotripsy for Treatment of Calcified Nodules,” we sat down with Dr. Ali, to learn more about this topical debate within the interventional community and separate the current perceived myths from the actual clinical evidence as it exists today in the treatment of calcified nodules.
Myth: Calcified nodules present most often in isolation
Clinical Evidence:
Although our eyes tend to focus on the “boulder” within the lumen of the coronary angiogram, in fact calcified nodules manifest in the presence of extensive severe calcification. Our data suggest that the burden of calcification is 4-fold higher in the presence of a nodule compared to without. In this regard it’s helpful to remember how calcified nodules actually form. As lipidic plaque accumulates within the artery wall, at a critical point the center of the lipid is so displaced from nutrient blood, that it develops into a necrotic core. To maintain vascular homeostasis, as a defense mechanism, the immune system can wall off the necrotic core by inducing calcification. This is one of the reasons that calcified nodules tend to occur in the proximal vessel – because the artery is large enough to accommodate a large lipid content through positive remodeling. This, now calcified former necrotic core, can either erupt into the vessel if the calcium is broken due to vessel torsion and bending, or simply protrude as the nodule becomes large enough or is pushed into the lumen by further lipid accumulation.
Myth: All calcified nodules are the same
Clinical Evidence:
Broadly speaking there are two types of calcified nodules. Eruptive calcified nodules, which are biologically active, and, protruding calcified nodules which are biologically inert. This is more than semantics, as the two types of nodules behave completely differently.
Eruptive calcified nodules “erupt” into the artery wall when a sheet of calcium breaks due to torsion, rotation and bending of the artery wall. Analogous to a glass in a bag, when the sheet calcium breaks some of the shards erupt into the vessel wall. These eruptions, which induce turbulent flow, and are devoid of endothelium, act as a nidus for thrombus formation causing up to 5% of all acute coronary syndromes.1
Protruding calcified nodules on the other hand, are as the name describe protrusions into the vessel wall. Analogous to a marbles in a bag, these protrusions either slowly grow into the lumen as they calcify or are pushed into the lumen by underlying lipid as lipid burden increases. While these protrusions can cause turbulent flow, they are covered by a fibrous cap and thus presumably endothelium, which does not induce thrombosis.
While these two different types of nodules are angiographically indistinguishable, intravascular imaging, in particular OCT, can help determine whether a nodule is eruptive or protruding. Recognizing this has direct clinical impact, as the response to therapy and the long term clinical outcomes of these two phenotypes is markedly different.
Myth: Atherectomy is the ideal tool for modifying nodular calcium
Clinical Evidence:
While it intuitively makes sense that shaving the nodule, or part thereof, would lead to the best acute result, data to support this theory is completely lacking. The only data to date comparing RA in calcified nodules versus non-nodular calcium showed a 3-fold higher clinically driven TLR at 5 years.2
As a parallel, treatment of calcified nodules with atherectomy could be compared to treatment of thrombus with aspiration catheters. While it intuitively makes sense, the volume of thrombus removed by aspiration has been shown to be less than 20%.3 Likewise, atherectomy only modifies a small proportion of the nodule, leaving the majority of the nodule, including the deep component unmodified. Moreover, because calcified nodules tend to occur in larger parts of the artery, the atherectomy may not impact the surrounding calcium due to wire-bias. On the contrary IVL, modifies the nodule by breaking it up into progressively smaller pieces with successive therapies. Moreover, since the IVL is wire-bias independent, it modifies not only the nodule itself, but the surrounding calcium, liberating circumferential vascular compliance.
The proof really is in the pudding. In our recent publication in JACC Intervention, we showed that the MSA, MLA and stent expansion were the same in severely calcified coronary arteries with or without nodular disease.4 That coupled with our recent CRT presentation, showing that the clinical outcomes comparing these two groups was similar, provides the strongest evidence base for interventional therapy of calcified nodules.
Myth: Nodular calcium is superficial; you just need to shave it off
Clinical Evidence:
Unfortunately, neither angiography, IVUS or OCT have the ability to determine the thickness of nodular calcium. Angiography lacks resolution, sound waves from IVUS reflect off the calcium, and OCT light is attenuated in the presence of very deep calcium or lipid. However, both conventional CT and micro-CT show that nodular calcification is deep. Pathophysiologically, by definition, nodular calcification has a deep component. As I mentioned earlier, nodules develop from necrotic core that progressively calcify, and necrotic cores only occur with positive remodeling vessel expansion and large lipid burdens.
Myth: Good, circumferential stent expansion with full apposition in calcified lesions equals a successful outcome
Clinical Evidence:
Again, while intuitively it makes sense that a circular stent would be optimal to restore vascular homeostasis, evidence to support this dogma is lacking. On the contrary neither eccentric stent expansion nor malapposition have been shown to impact clinical outcomes in DES. Blood really doesn’t care whether it goes through a circle or an oval, or behind a strut, or inside a strut. Rather, the most important determinant of long-term PCI outcome is the MSA. In keeping with this, in our recent publication in JACC Intervention, we showed that the MSA, MLA and stent expansion were the same in severely calcified coronary arteries with or without nodular disease. That coupled with our recent CRT presentation, showing that the clinical outcomes comparing these two groups was similar, provides the strongest evidence base for interventional therapy of calcified nodules.
Myth: A good acute outcome with calcified nodules is indicative of sustainable long-term outcomes
Clinical Evidence:
Sadly not. In a very recent analysis published in JACC Intervention we showed that the calcified nodule phenotype heavily impacts the long-term clinical outcome.5 Despite a better acute stent expansion in eruptive calcified nodules, this phenotype has a 4-fold higher risk of TLF compared to protruding nodules, reaching a 20% event rate at 2 years. It appears as though the mechanism by which the eruptive nodules fail, is a re-protrusion through the stent struts over time. Thus far we have not been able to determine which nodules are most likely to re-protrude other than those at hinge points in the vessel. Moreover, what treatment modality is optimal to prevent this re-protrusion remains unknown.
Myth: We know which treatment strategy is the ideal approach for calcific nodules today
Clinical Evidence:
What we do know is that the safety and effectiveness of IVL now with 2yr f/u in these patients is encouraging. But, there is still a lot we need to learn. Research in this area has been hampered by the prevalence of calcified nodules. Approximately 5-10% of severely calcified coronary lesions have a calcified nodule.6 Given this relatively low prevalence, it has proven challenging to perform prospective controlled studies. We need more real-world data in nodules across calcium arcs with intravascular imaging to start to determine the optimal algorithm for treatment of calcified nodules, such that we can improve both short and long term PCI outcomes. Certainly, the IVL data is encouraging and definitely proves a role for IVL in treatment of calcified nodules. Whether concomitant atherectomy may alter the plaque phenotype to facilitate more calcium fracture and lesion modification is certainly an interesting and valid hypothesis. We have embarked on a prospective study to evaluate this hypothesis, and hope to provide insight in the next few years.
- 1. Pengchata, P. et al. (2023). Characteristics and Pattern of Calcified Nodule and/or Nodular Calcification Detected by Intravascular Ultrasound on the Device-Oriented Composite Endpoint (DoCE) in Patients with Heavily Calcified Lesions Who Underwent Rotational Atherectomy-Assisted Percutaneous Coronary Intervention. Journal of Interventional Cardiology, 2023, 1–14. https://doi.org/10.1155/2023/6456695
- 2. Morofuji, T. et al. (2021). Clinical impact of calcified nodule in patients with heavily calcified lesions requiring rotational atherectomy. Catheterization and Cardiovascular Interventions, 97(1), 10–19. https://doi.org/10.1002/ccd.28896
- 3. Bhindi, R. et al. (2015). Culprit lesion thrombus burden after manual thrombectomy or percutaneous coronary intervention-alone in ST-segment elevation myocardial infarction: the optical coherence tomography sub-study of the TOTAL (ThrOmbecTomy versus PCI ALone) trial. European Heart Journal, 36(29), 1892–1900. https://doi.org/10.1093/eurheartj/ehv176
- 4. Ali, Z. A., et al. (2023). Safety and effectiveness of coronary intravascular lithotripsy for treatment of calcified nodules. JACC: Cardiovascular Interventions. https://doi.org/10.1016/j.jcin.2023.02.015
- 5. Sato T. et al. (2023). Impact of Eruptive vs Noneruptive Calcified Nodule Morphoplogy on Acuet and Long-Term Outcomes After Stenting. JACC: Cardiovascular Interventions. In Press.
- 6. Petrossian, G., et al. (2022). Role of Intracoronary Imaging in Acute Coronary Syndromes. US Cardiology Review, 16. https://doi.org/10.15420/usc.2022.03
To learn more about the impact of Shockwave IVL on nodular calcium, follow us on Twitter @ShockwaveIVL.
Coronary Important Safety Information:
In the United States: Rx only.
Indications for Use—The Shockwave Intravascular Lithotripsy (IVL) System with the Shockwave C2 Coronary IVL Catheter is indicated for lithotripsy-enabled, low-pressure balloon dilatation of severely calcified, stenotic de novo coronary arteries prior to stenting.
Contraindications—The Shockwave C2 Coronary IVL System is contraindicated for the following: This device is not intended for stent delivery. This device is not intended for use in carotid or cerebrovascular arteries.
Warnings— Use the IVL Generator in accordance with recommended settings as stated in the Operator’s Manual. The risk of a dissection or perforation is increased in severely calcified lesions undergoing percutaneous treatment, including IVL. Appropriate provisional interventions should be readily available. Balloon loss of pressure was associated with a numerical increase in dissection which was not statistically significant and was not associated with MACE. Analysis indicates calcium length is a predictor of dissection and balloon loss of pressure. IVL generates mechanical pulses which may cause atrial or ventricular capture in bradycardic patients. In patients with implantable pacemakers and defibrillators, the asynchronous capture may interact with the sensing capabilities. Monitoring of the electrocardiographic rhythm and continuous arterial pressure during IVL treatment is required. In the event of clinically significant hemodynamic effects, temporarily cease delivery of IVL therapy.
Precautions— Only to be used by physicians trained in angiography and intravascular coronary procedures. Use only the recommended balloon inflation medium. Hydrophilic coating to be wet only with normal saline or water and care must be taken with sharp objects to avoid damage to the hydrophilic coating. Appropriate anticoagulant therapy should be administered by the physician. Precaution should be taken when treating patients with previous stenting within 5mm of target lesion.
Potential adverse effects consistent with standard based cardiac interventions include– Abrupt vessel closure – Allergic reaction to contrast medium, anticoagulant and/or antithrombotic therapy-Aneurysm-Arrhythmia-Arteriovenous fistula-Bleeding complications-Cardiac tamponade or pericardial effusion-Cardiopulmonary arrest-Cerebrovascular accident (CVA)-Coronary artery/vessel occlusion, perforation, rupture or dissection-Coronary artery spasm-Death-Emboli (air, tissue, thrombus or atherosclerotic emboli)-Emergency or non-emergency coronary artery bypass surgery-Emergency or non-emergency percutaneous coronary intervention-Entry site complications-Fracture of the guide wire or failure/malfunction of any component of the device that may or may not lead to device embolism, dissection, serious injury or surgical intervention-Hematoma at the vascular access site(s)-Hemorrhage-Hypertension/Hypotension-Infection/sepsis/fever-Myocardial Infarction-Myocardial Ischemia or unstable angina-Pain-Peripheral Ischemia-Pseudoaneurysm-Renal failure/insufficiency-Restenosis of the treated coronary artery leading to revascularization-Shock/pulmonary edema-Slow flow, no reflow, or abrupt closure of coronary artery-Stroke-Thrombus-Vessel closure, abrupt-Vessel injury requiring surgical repair-Vessel dissection, perforation, rupture, or spasm.
Risks identified as related to the device and its use: Allergic/immunologic reaction to the catheter material(s) or coating-Device malfunction, failure, or balloon loss of pressure leading to device embolism, dissection, serious injury or surgical intervention-Atrial or ventricular extrasystole-Atrial or ventricular capture.
Prior to use, please reference the Instructions for Use for more information on warnings, precautions and adverse events. https://shockwavemedical.com/IFU
Please contact your local Shockwave representative for specific country availability and refer to the Shockwave C2 and C2+ instructions for use containing important safety information.